Following the successful return of spontaneous circulation (ROSC) after a cardiac arrest, the focus of treatment transitions from the immediate resuscitation phase to comprehensive post-cardiac arrest care. This critical phase, guided by the Pediatric Advanced Life Support (PALS) guidelines, employs a systematic approach to stabilize the patient and optimize outcomes. The core objective is to mitigate morbidity and mortality by meticulously managing the respiratory, cardiovascular, and neurologic systems.
The post-cardiac arrest phase emphasizes a structured evaluate, identify, intervene sequence, moving away from the cardiac arrest algorithm and towards a systematic approach algorithm. This shift is crucial for addressing the underlying causes and consequences of cardiac arrest, ensuring a holistic and system-based recovery process.
The primary goals of post-cardiac arrest care center around the prompt recognition and effective treatment of organ system dysfunction. Optimization of oxygenation, ventilation, and perfusion are paramount to stabilize cardiopulmonary function and, critically, to preserve neurologic function.
Systematic Approach Diagram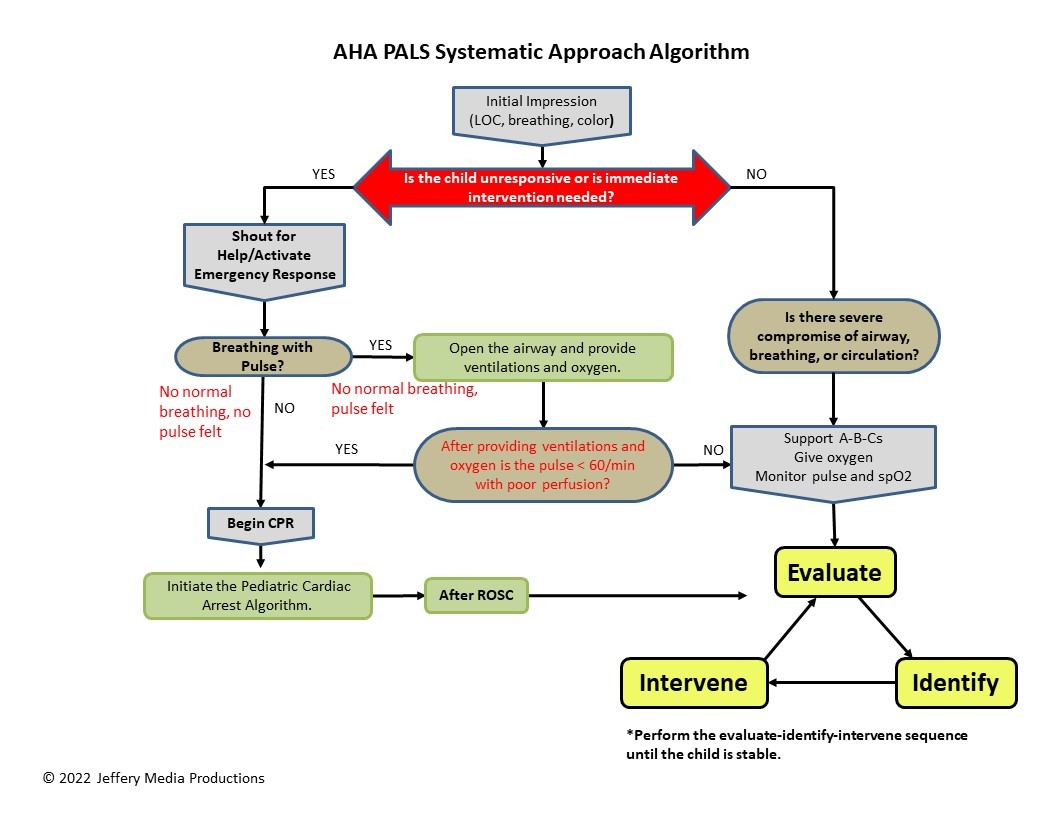 PALS Systematic Approach Algorithm Diagram for Post-Cardiac Arrest Care
PALS Systematic Approach Algorithm Diagram for Post-Cardiac Arrest Care
Respiratory System Goals and Interventions
The immediate priorities within the respiratory system post-cardiac arrest are to secure and stabilize the airway, optimize oxygenation, and ensure adequate ventilation.
Goals:
- Achieve and maintain optimal airway patency.
- Ensure adequate oxygenation to meet tissue demands.
- Provide effective ventilation to manage carbon dioxide levels.
Interventions:
- Confirm Endotracheal Tube (ET) Placement: If intubation was performed, verify correct placement through auscultation, capnography, and chest X-ray if needed.
- Oxygenation and Ventilation Support: Administer supplemental oxygen to achieve appropriate oxygen saturation levels. Mechanical ventilation may be necessary to support breathing and manage CO2 levels, guided by blood gas analysis.
Assessments:
- End-Tidal CO2 (Capnography) Monitoring: Continuously monitor ETCO2 to assess ventilation effectiveness.
- Blood Gas Analysis: Regularly evaluate arterial or venous blood gases to assess oxygenation, ventilation, and acid-base balance.
- Chest X-ray: Obtain a chest X-ray to confirm ET tube placement and evaluate for any pulmonary pathology.
Cardiovascular System Goals and Interventions
Supporting cardiovascular function and tissue perfusion is crucial in the post-cardiac arrest phase to prevent shock and secondary organ damage.
Goals:
- Maintain adequate blood pressure to ensure organ perfusion.
- Support cardiovascular function to optimize cardiac output.
- Prevent and manage shock states.
Interventions:
- Blood Pressure and Perfusion Management: Administer intravenous fluids and vasoactive medications as needed to maintain adequate blood pressure and tissue perfusion.
- Arrhythmia Treatment: Identify and treat any post-arrest arrhythmias promptly as they can compromise hemodynamic stability.
Assessments:
- Tissue Perfusion Markers: Monitor lactate levels, venous oxygen saturation (ScvO2), and base deficit as indicators of tissue perfusion adequacy.
- Hemodynamic Monitoring: Utilize intra-arterial blood pressure monitoring for continuous and precise blood pressure assessment.
- Clinical Perfusion Assessment: Regularly evaluate urine output, capillary refill time, and skin temperature to assess peripheral perfusion.
Neurologic System Goals and Interventions
The neurologic system is particularly vulnerable after cardiac arrest. The primary goal is to maximize the potential for neurologically intact survival.
Goals:
- Promote neurologic recovery and minimize brain injury.
- Prevent secondary neurologic insults.
Interventions:
- Targeted Temperature Management (TTM): Implement TTM to improve neurologic outcomes. This typically involves cooling the patient to a specific target temperature for a defined period.
- Fever Prevention: Actively prevent hyperthermia as it can worsen neurologic injury.
- Analgesia and Sedation: Provide adequate analgesia and sedation to reduce metabolic demand and prevent agitation, while being mindful of neurologic assessment.
- Seizure Management: Promptly identify and treat seizures, which are common post-cardiac arrest.
- Intracranial Pressure (ICP) Management: Monitor for and manage signs of increased ICP, avoiding hyperventilation which can be detrimental.
Assessments:
- Core Temperature Monitoring: Continuously monitor core body temperature, especially during TTM.
- Point-of-Care Blood Glucose: Regularly check and manage blood glucose levels as hypo- and hyperglycemia can negatively impact neurologic outcomes.
- Ongoing Neurological Assessments: Perform serial neurologic examinations to monitor neurologic status and identify any changes.
Post-cardiac arrest care in PALS is a dynamic and multifaceted process. By systematically addressing the respiratory, cardiovascular, and neurologic systems, healthcare providers can significantly improve the chances of survival and neurological recovery in pediatric patients following cardiac arrest. This structured approach ensures that all critical aspects of post-resuscitation stabilization are meticulously considered and managed.